Abstract
Purpose. To quantify the contribution of distributional processes across the blood-brain barrier (BBB) to the delay in antinociceptive effect of morphine in rats.
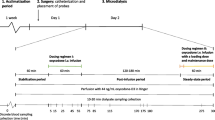
Methods. Unbound morphine concentrations were monitored in venous blood and in brain extracellular fluid (ECF) using microdialysis (MD) and in arterial blood by regular sampling. Retrodialysis by drug was used for in vivo calibration of the MD probes. Morphine was infused (10 or 40 mg/kg) over 10 min intravenously. Nociception, measured by the electrical stimulation vocalisation method, and blood gas status were determined.
Results. The half-life of unbound morphine in striatum was 44 min compared to 30 min in venous and arterial blood (p < 0.05). The BBB equilibration of morphine, expressed as the ratio of areas under the curve between striatum and venous blood, was less than unity (0.28 ± 0.09 and 0.22 ± 0.17 for 10 and 40 mg/kg), respectively, indicating active efflux of morphine across the BBB. The concentration-effect relationship exhibited a clear hysterisis with an effect delay half-life of 32 and 5 min based on arterial blood and brain ECF concentrations, respectively.
Conclusions. Eighty five percent of the effect delay was caused by morphine transport across the BBB, indicating possible involvement of rate limiting mechanisms at the receptor level or distributional phenomena for the remaining effect delay of 5 min.
Similar content being viewed by others
REFERENCES
A. Mansour and S. J. Watson. Anatomical distribution of opioid receptors in mammalians: An overview. In H. Akil and E.J. Simon (eds), Opioids I, Springer-Verlag, Berlin, 1993, pp. 79–102.
B. E. Dahlström and L. K. Paalzow. Pharmacokinetics of morphine in plasma and discrete areas of the rat brain. J. Pharmacokinet. Biopharm. 3:293–302 (1975).
B. E. Dahlström, L. K. Paalzow, G. Segre, and A. J. Ågren. Relation between morphine pharmacokinetics and analgesia. J.Pharmacokinet. Biopharm. 6:41–53 (1978).
M. Gårdmark, M. Ekblom, R. Bouw, and M. Hammarlund-Udenaes. Quantification of effect delay and acute tolerance development to morphine in the rat. J. Pharmacol. Exp. Ther. 267: 1061–1067 (1993).
W. H. Oldendorf, S. Hyman, L. Braun, and S. Z. Oldendorf. Blood-brain barrier: Penetration of morphine, codeine, heroin, and methadone after carotid injection. Science 178:984–986 (1972).
T. A. Aasmundstad, J. Morland, and R. E. Paulsen. Distribution of morphine 6-glucuronide and morphine across the blood-brain barrier in awake, freely moving rats investigated by in vivo microdialysis sampling. J. Pharmacol. Exp. Ther. 275:435–441 (1995).
U. Bickel, O. P. Schumacher, Y. S. Kang, and K. Voigt. Poor permeability of morphine 3-glucuronide and morphine 6-glucuronide through the blood-brain barrier in the rat. J Pharmacol Exp Ther. 278:107–113 (1996).
D. Wu, Y. S. Kang, U. Bickel, and W. M. Pardridge. Blood-brain barrier permeability to morphine-6-glucuronide is markedly reduced compared with morphine. Drug Metab Dispos. 25:768–771 (1997).
E. C. M. de Lange, M. Danhof, A. G. de Boer, and D. D. Breimer. Methodological considerations of intracerebral microdialysis in pharmacokinetic studies on drug transport across the blood-brain barrier. Brain. Res. Rev. 25:27–49 (1997).
W. F. Elmquist and R. J. Sawchuk. Application of microdialysis in pharmacokinetic studies. Pharm. Res. 14:267–288 (1997).
Y. Wang and D. F. Welty. The simultaneous estimation of the influx and efflux blood-brain barrier permeabilities of gabapentin using a microdialysis-pharmacokinetic approach. Pharm Res. 13: 398–403 (1996).
M. Hammarlund-Udenaes, L. K. Paalzow, and E. C. M. de Lange. Drug equilibration across the blood-brain barrier–Pharmacokinetic considerations based on the microdialysis method. Pharm. Res. 14:128–134 (1997).
L. K. Paalzow. Measurement and modeling analgesic drug effect. In C. J. van Boxtel, N. H. G. Holford, and M. Danhof (eds), The in vivo study of drug action–Principles and applications of kinetic-dynamic modelling, Elsevier Science Publishers B.V., Amsterdam, 1992, pp. 133–153.
M. R. Bouw and M. Hammarlund-Udenaes. Methodological aspects of the use of a calibrator in in vivo microdialysis–further development of the retrodialysis method. Pharm. Res. 15:1673–1679 (1998).
M. N. Carroll and R. K. S. Lim. Observation on the neuropharmacology of morphine and morphinelike analgesia. Arch. Int. Pharmacodyn. Ther. 125:383–403 (1960).
M. Ekblom, M. Gårdmark, and U. M. Hammarlund. Estimation of unbound concentrations of morphine from microdialysate concentrations by use of nonlinear regression analysis in vivo and in vitro during steady state conditions. Life Sci. 51:449–460 (1992).
S. L. Beal and L. S. Sheiner. NONMEM user's guide. NONMEM Project Group, 1992, University of California at San Francisco: San Francisco.
E. N. Jonsson and M. O. Karlsson. Xpose–An S-PLUS based population pharmacokinetic/pharmacodynamic model building aid for NONMEM. Comput. Methods Programs Biomed. 58:51–64 (1999).
L. B. Sheiner, D. R. Stanski, S. Vozeh, R. D. Miller, and J. Ham. Simultaneous modeling of pharmacokinetics and pharmacodynamics: Application to d-tubocurarine. Clin. Pharmacol. Ther. 25: 358–371 (1979).
G. Skopp, L. Potsch, B. Ganssmann, R. Aderjan, and R. Mattern. A preliminary study on the distribution of morphine and its glucuronides in the subcompartments of blood. J Anal Toxicol. 22: 261–264 (1998).
R. Xie, M. Hammarlund-Udenaes, A. G. de Boer, and E. C. de Lange. The role of P-glycoprotein in blood-brain barrier transport of morphine: Transcortical microdialysis studies in mdr1a (-/-) and mdr1a (+/+) mice. Br. J. Pharmacol. 128:563–568 (1999).
M. Ekblom, M. Hammarlund-Udenaes, and L. K. Paalzow. Modeling of tolerance development and rebound effect during different intravenous administrations of morphine to rats. J. Pharmacol. Exp. Ther. 266:244–252 (1993).
D. M. Ouellet and G. M. Pollack. Pharmacodynamics and tolerance development during multiple intravenous bolus morphine administration in rats. J. Pharmacol. Exp. Ther. 281:713–720 (1997).
D. M. Ouellet and G. M. Pollack. Effect of prior morphine-3-glucuronide exposure on morphine disposition and antinociception. Biochem Pharmacol. 53:1451–1457 (1997).
S. P. Letrent, G. M. Pollack, K. R. Brouwer, and K. L. Brouwer. Effect of GF120918, a potent P-glycoprotein inhibitor, on morphine pharmacokinetics and pharmacodynamics in the rat. Pharm. Res. 15: 599–605 (1998).
M. Gårdmark, A. U. Höglund, and M. Hammarlund-Udenaes. Aspects on tail-flick, hot-plate and electrical stimulation tests for morphine antinociception. Pharmacol. Toxicol. 83:252–258 (1998).
S. P. Letrent, G. M. Pollack, K. R. Brouwer, and K. L. Brouwer. Effects of a potent and specific P-glycoprotein inhibitor on the blood-brain barrier distribution and antinociceptive effect of morphine in the rat. Drug. Metab. Dispos. 27:827–834 (1999).
F. Stain, M. J. Barjavel, P. Sandouk, M. Plotkine, J. M. Scherrmann, and H. N. Bhargava. Analgesic response and plasma and brain extracellular fluid pharmacokinetics of morphine and morphine-6-beta-D-glucuronide in the rat. J. Pharmacol. Exp. Ther. 274(2): 852–857 (1995).
Y. Wang and R. J. Sawchuk. Zidovudine transport in the rabbit brain during intravenous and intracerebroventricular infusion. J. Pharm. Sci. 84:871–876 (1995).
C. K. Kuo, N. Hanioka, Y. Hoshikawa, K. Oguri, and H. Yoshimura. Species difference of site-selective glucuronidation of morphine. J. Pharmacobio-Dyn. 14:187–193 (1991).
M. Ekblom, M. Gårdmark, and M. Hammarlund-Udenaes. Pharmacokinetics and pharmacodynamics of morphine-3-glucuronide in rats and its influence on the antinociceptive effect of morphine. Biopharm. Drug Disp. 14:1–11 (1993).
M. Gårdmark, M. O. Karlsson, F. Jonsson, and M. Hammarlund-Udenaes. Morphine-3-glucuronide has a minor effect on morphine antinociception. Pharmacodynamic modeling. J. Pharm. Sci. 87:813–820 (1998).
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Bouw, M.R., Gårdmark, M. & Hammarlund-Udenaes, M. Pharmacokinetic-Pharmacodynamic Modelling of Morphine Transport Across the Blood-Brain Barrier as a Cause of the Antinociceptive Effect Delay in Rats—A Microdialysis Study. Pharm Res 17, 1220–1227 (2000). https://doi.org/10.1023/A:1026414713509
Issue Date:
DOI: https://doi.org/10.1023/A:1026414713509