Abstract
Background
This study aimed to compare single-port transumbilical total laparoscopic hysterectomy (SPLS-TLH) and four-port total laparoscopic hysterectomy (TLH) in terms of postoperative pain.
Methods
The study enrolled 68 patients who underwent TLH from October 2009 to March 2010 and randomly assigned them to one of two groups. Patient demographics, operative outcomes, and postoperative pain were prospectively examined.
Results
Four cases in the SPLS-TLH group were converted to other laparoscopic approaches. The two study groups did not differ in terms of patient demographics and surgical outcomes. Postoperative pain scores, measured using a visual analog scale, did not differ between the two groups. However, significantly higher total requests for analgesics were observed in the SPLS-TLH group (11.3 ± 4.1 vs. 7.7 ± 2.7; p < 0.001).
Conclusion
Compared with four-port TLH, SPLS-TLH is a feasible approach with comparable operative outcomes. However, reduction of postoperative pain is not evident with SPLS-TLH.
Similar content being viewed by others
Hysterectomy is one of the most commonly performed gynecologic surgeries. The Nationwide Inpatient Sample of the Healthcare Cost and Utilization Project reported that in the Unites States, 538,722 cases of hysterectomies were performed for benign gynecologic disease in 2003 [1]. The laparoscopic approach for hysterectomy has several advantages such as reduced pain, faster recovery, better cosmetic results, cost effectiveness, and shorter hospital stay compared with an abdominal approach [2]. To maximize these benefits of laparoscopic procedures, various efforts have been made including the reduction of port size and port number. Recently, single-port transumbilical laparoscopic surgery (SPLS) has been introduced as a result of these efforts.
The SPLS procedure requires only one incision at the umbilicus, avoiding operative complications such as epigastric vessel injury, operative wound infection, and visceral organ damage, which are associated with making additional punctures for ancillary ports. Actually, SPLS was introduced as early as the 1970s. Gynecologists performed laparoscopic tubal ligations with Yoon’s rings through a single transumbilical incision.
In 1991, Pelosi and Pelosi [3] performed laparoscopic hysterectomy using a single puncture. However, the technical difficulties prevented the procedure from becoming more popular in the field of gynecologic surgery. Since then, laparoscopic instrumentation and technique have considerably advanced, and the potential benefits of SPLS such as better cosmetic results, less postoperative pain, faster recovery, and reduced operative complications have gained more attention from gynecologic surgeons [4–6].
The authors demonstrated in a previous report that SPLS is a feasible approach for total laparoscopic hysterectomy (TLH) in terms of surgical outcomes [7]. Despite the surgical feasibility, technical difficulty performing hysterectomy remains an obstacle to the widespread use of SPLS. The benefit of SPLS-TLH should be verified before it is recommended to gynecologists. From the patient’s perspective, reducing the pain related to surgery is one of the greatest concerns. Therefore, the current study was performed to evaluate the benefit of SPLS-TLH compared with conventional TLH in terms of postoperative pain.
Materials and methods
Patients referred to the Division of Gynecologic Oncology, Department of Obstetrics and Gynecology at Severance Hospital, a tertiary teaching and research institution in Seoul, Korea, who had an indication for hysterectomy between October 2009 and March 2010 were invited to participate in the study. This study was approved by the Institutional Review Board (IRB) of Yonsei University College of Medicine (IRB #4-2009-0364) before enrollment of patients in the study. Written informed consent was obtained from both the patient and her legal guardian before enrollment.
The eligibility criteria for the patients specified an age of 20 years or older, no evidence of gynecologic malignancy on imaging studies, normal cervical cytology or histologically proven preinvasive cervical neoplasia, CA-125 of 150 IU/ml or less, appropriate medical status for laparoscopic surgery (American Society of Anesthesiologists Physical Status classification system 1 or 2), and adequate uterus size for vaginal removal (≤12 gestational weeks size by pelvic examination).
The exclusion criteria ruled out a uterine size larger than 12 gestational weeks by pelvic examination, history of pelvic radiation therapy, suspicion of gynecologic cancer, and more than three prior laparotomies. Patients who had been treated for gastrointestinal or gynecologic malignancy also were excluded from the study.
All the procedures were performed by three skilled surgeons (Y.T.K., S.W.K., E.J.N.) with the assistance of a gynecologic oncology fellow and a chief resident. All three surgeons had the ability to perform laparoscopically assisted radical hysterectomy and endometrial cancer-staging surgery. In addition, they had managed more than 100 cases of conventional TLH and 30 cases of single-port laparoscopic surgery.
All the patients in both groups underwent a type 4 E total laparoscopic hysterectomy according to the American Association of Gynecologic Laparoscopists classification. We used a Ligasure system (Covidien, Valleylab, Boulder, CO) to divide the utero-ovarian ligaments (or infundibulo-pelvic ligaments) and round ligaments. The broad ligaments were dissected with a monopolar L-hook. The vesico-uterine peritoneal fold was opened, and the bladder was mobilized with a monopolar hook until the anterior vagina was identified.
To seal and divide the uterine vessels, the Ligasure system and bipolar electrocautery were used. Most of the patients who underwent TLH had a relatively small uterus. It was not difficult to extract the resected uterus through the vagina. For the patients who required morcellation for removal of the uterus, we performed wedge morcellation.
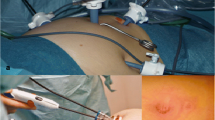
The vaginal vault was sutured laparoscopically or transvaginally depending on the surgeon’s decision. Regardless of the approach for vault repair, we made four simple interrupted sutures with 0 Polysorb for vaginal vault closure. The surgical procedures were identical in the two groups except for the use of the Ligasure system in the SPLS group. For the SPLS patients, a 1.2-cm vertical intraumbilical skin incision was made, and a 1.5-cm rectus fasciotomy was performed for entrance to the peritoneal cavity. The authors made a single three-channel port using the Alexis wound retractor (Applied Medical, Rancho Santa Margarita, CA) and a surgical glove, as reported in a previous study [7].
For conventional TLH, four 5-mm trocars were placed in the abdomen. A 5-mm port for the laparoscope was inserted through the umbilicus. Two 5-mm ports were placed in the left lower quadrant of the abdomen and one in the right lower quadrant. In both groups, a rigid 30°, 5-mm laparoscope was used.
The authors did not use any articulating instruments for SPLS. A Foley catheter was inserted to drain the bladder. A RUMI uterine manipulator (Cooper surgical Inc., Trumbull, CT) was placed with a KOH Colpotomizer system (Cooper Surgical Inc., Trumbull, CT). All the patients received prophylactic antibiotics 30 min before the procedure.
The patients’ demographic information, operative outcomes, and operative complications were prospectively collected by three gynecologic oncology fellows (Y.W.J, S.H.L., J.H.P.). The total operative time was defined as the time from the beginning of the skin incision to the completion of the skin closure. Although estimated blood loss (EBL) was calculated by the difference in the total amounts of suctioned and irrigation fluids, it was difficult to measure exactly in many cases due to little operative bleeding. Therefore, the authors evaluated hemoglobin on postoperative day (POD) 1 and POD 3.
Postoperative pain was measured by a second-year resident (H.Y.K.). Postoperative pain intensity was rated with the patient at rest by using a visual analog scale (VAS). The scale was presented as a 10-cm line with verbal descriptors anchored using “no pain” and “worst imaginable pain.”
To compare the postoperative pain between the SPLS-TLH group and the conventional TLH group, the authors devised a standard protocol for pain management and examined several parameters related to pain. General anesthesia was induced with intravenous (IV) propofol (2 mg/kg) during preoxygenation with 100% oxygen via a facial mask. After consciousness was confirmed, assisted ventilation was started with sevoflurane, and continuous IV infusion of remifentanil (1.5 μg/kg) was started. Intravenous fentanyl (50 μg) was given to patients 10 min before the surgery was completed. At the end of surgery, the IV infusion of remifentanil was stopped. Before the patients left the postanesthesia care unit, IV fentanyl (50 μg) was administered once more.
To manage postoperative pain in a general ward, the authors used only three types of analgesics, namely, ketorolac 30 mg injected intramuscularly (IM), pethidine HCl 25 mg injected IM, and a nonsteroidal antiinflammatory drug (taniflumate 370 mg) administered orally. Pethidine HCl was used only when the patient had a pain exceeding 7 on the VAS scale. In other cases, ketorolac 30 mg was injected IM as the primary analgesic. After a soft diet was permitted, taniflumate 370 mg was administered three times daily as the primary analgesic medication if there was no demand for other analgesics from the patient.
All the patients received an IM injection of ketorolac 30 mg when they returned to the ward after surgery. We recorded the time at which the patient requested the second dose of analgesics. In addition, we measured the total requests for analgesics used during the postoperative hospitalization period. Patients were asked to rate their pain intensity 6 h after surgery, and at 7 a.m. on PODs 1, 2, and 3.
This study was designed as a randomized prospective study to examine whether postoperative pain differed significantly between single-port surgery and conventional laparoscopic procedures for patients who underwent hysterectomy. The primary end point of the study was postoperative pain, measured at 6 h after the patient’s return to the ward from the recovery unit. The secondary end point was operative time. The sample size was calculated based on the difference in pain intensity measured 6 h after the surgery, collected retrospectively for patients who underwent single port hysterectomy and conventional TLH at our hospital before this study.
A difference of 0.8 in the VAS score was considered clinically relevant. Type 1 and 2 errors were set to the usual levels of 0.05 and 0.20, respectively. Assuming a 10% withdrawal rate, the number of cases needed per group was approximately 34. Randomization was based on computer-generated random sampling numbers. Codes were maintained by a coordinator (J.A.R.) until immediately before use.
A Kolmogorov–Smirnov test was performed for normality. Continuous comparative data with a normal distribution were analyzed using Student’s t-test, whereas those not consistent with a normal distribution were analyzed using the Mann–Whitney U test. Discrete variables were compared using the chi-square test, and Fisher’s exact test was used when the expected count in any cell was less than five. A difference was considered significant when the p value was less than 0.05. The statistical software package PASW statistics 17.0 (SPSS Inc., Chicago, IL) was used for all data analyses.
Results
Between October 2009 and March 2010, 110 patients underwent laparoscopic hysterectomy. Of these 110 patients, 68 who met the inclusion criteria were enrolled in the study as the authors planned (Fig. 1). No conversion to laparotomy occurred in either group. However, four patients assigned to the single-port surgery group underwent conversion to some other laparoscopic approach. One patient with a diagnosis of granulosa cell tumor during the surgery underwent conversion to a two-port laparoscopic staging surgery. Two patients underwent four-port laparoscopic TLH due to severe pelvic adhesion and large uterus size. Their uteri weighed respectively 353 and 280 g. One patient with a 180-g uterus had a bladder injury during single-port surgery and thus was converted to the two-port approach. These four patients were excluded from the analysis of the patient demographics and operative outcomes including pain because placement of additional ports in the abdomen would affect postoperative pain.
Table 1 shows the demographics of the patients. Although no significant difference is presented (p = 0.185), the specimen weight for the single-port surgery group was lighter than for the four-port group. This may have been due to the four cases excluded from analysis in the single-port surgery group. The two groups did not differ significantly in terms of patient characteristics and were comparable in terms of preoperative diagnoses.
The surgical results also were compared between the two groups (Table 2). The patients in the single-port surgery group experienced slightly longer operative times than the four-port group, but the difference was not statistically significant (89.1 ± 25.4 vs. 80.1 ± 27.1; p = 0.175). A higher proportion of the patients underwent the transvaginal approach for vaginal vault repair in the single-port group (p = 0.001).
To analyze intraoperative complications, the authors included the four patients who underwent conversion from single-port surgery to a two- or four-port approach. In 68 cases of TLH, 1 patient in the single-port group experienced a bladder injury. The authors made one more puncture in the suprapubic area and laparoscopically repaired the injured bladder with 2-0 Vicryl. One patient in the single-port group received a transfusion because of postoperative anemia. Postoperative fever more frequently developed in patients who underwent single-port surgery than in patients who underwent the four-port approach, but the difference was not statistically significant (p = 0.071).
The postoperative pain scores were comparable between the two groups (Fig. 2). The postoperative pain scores at 6 h, the primary end point of the study, did not differ based on the laparoscopic method (p = 0.516) (Table 3). Ketorolac was more frequently requested by the patients in the single-port group (median, 5.0 vs. 3.5; p = 0.001). In addition, no statistically significant differences in the total amounts of analgesics were observed between the two groups (11.3 ± 4.1 in the single port group vs. 7.7 ± 2.7 in the four-port group; p < 0.001).
The vaginal vault was vaginally repaired in eight patients. The two vault repair methods did not show any difference in terms of postoperative pain (data not shown).
Discussion
The SPLS procedure has several disadvantages such as restricted movement of surgical instruments due to the proximity of the instruments and a lack of long-term follow-up data on the feasibility of umbilical incisions. Despite these weaknesses, the potential advantages of SPLS hold promise for patients. For this reason, several researchers, including the authors, have performed SPLS and demonstrated that SPLS in gynecologic surgery, including adnexal surgery, hysterectomy, and even pelvic lymphadenectomy, is a feasible approach [4, 5, 7, 8]. However, only a limited number of studies have demonstrated the possible advantages of SPLS over conventional laparoscopic surgery. The authors performed this randomized prospective study to examine whether SPLS has an advantage over four-port TLH in reducing postoperative pain.
The results of the study demonstrate that the single-port approach for performing TLH is comparable with the four-port approach in terms of surgical outcomes including operative times, EBL, and intraoperative complications. However, single-port TLH has no benefit in reduction of postoperative pain compared with four-port TLH.
It is difficult to compare exactly the pain related to certain procedures because pain is very subjective, and numerous factors are involved in postoperative pain. The VAS offers an easy way to measure subjective pain and is relatively sensitive in assessing acute pain after surgery. However, the VAS cannot evaluate the nature of pain other than its intensity. It is inadequate for assessment of chronic pain, which affects physical and social functions [9]. Therefore, the authors measured pain scores, the analgesic requirements of the patient, and the time that the patient made her first request for analgesics after she returned to the ward from the recovery unit in the usual clinical setting.
Our results showed that the total amount of analgesics differed between the two groups, although there were no differences in VAS pain scores at discrete time points nor in the time of the first request for analgesics. This discrepancy made it difficult for the authors to conclude which methods had a beneficial effect on patients with regard to procedure-related pain. However, it is reasonable to conclude that SPLS has no advantage over four-port laparoscopic hysterectomy in terms of postoperative pain.
Few reports are available for comparing results. Kim et al. [10] conducted a retrospective case-control study comparing the perioperative outcomes between single-port access, laparoscopically assisted vaginal hysterectomy (SPA-LAVH) and conventional vaginal hysterectomy (LAVH). The authors measured postoperative pain scores using a VAS and reported that pain scores measured 24 and 36 h after surgery (2.5 ± 0.7 vs. 3.5 ± 0.8; p < 0.01 and 1.7 ± 1.2 vs. 2.9 ± 1.1, p < 0.01, respectively) were lower with the single-port approach. They concluded that SPA-LAVH was associated with less postoperative pain.
Another comparative study was performed in the field of general surgery. Tsimoyiannis et al. [11] investigated pain scores in single-port laparoscopic cholecystectomy versus those in conventional laparoscopic cholecystectomy during a randomized controlled trial. Four trocars, including one 11-mm umbilical port and three 5-mm ports, were placed in the abdomen for conventional laparoscopic cholecystectomy. In the single-port cholecystectomy group, a single intraumbilical 12-mm incision was made, and three trocars were inserted through the umbilicus. The results of the study showed significantly less pain in the single-port surgery group than in the conventional group, especially for abdominal pain after the first postoperative 12 h: 12 h (1.80 ± 0.95 vs. 1.65 ± 0.67; p = 0.001), 24 h (1.55 ± 0.94 vs. 0.50 ± 0.60; p < 0.0001), 48 h (1.35 ± 0.74 vs. 0.20 ± 0.41; p < 0.0001), and 72 h (0.85 ± 0.67 vs. 0.05 ± 0.22; p < 0.0001).
Several reasons explain such discordance between results for postoperative pain comparisons. First, the placement of laparoscopic ports differed in conventional laparoscopy groups. We used four 5-mm ports, whereas Kim et al. [10] used one 12-mm trocar and two 5-mm trocars, and Tsimoyiannis et al. [11] made four punctures in the abdomen, using one 11-mm trocar and three 5-mm trocars. Several studies showed that either the size or the number of ports related to the degree of postoperative pain [12–14]. Therefore, the differences in both the size and the number of trocars may be a factor that caused disparity between the results.
Second, the differences in surgical procedures also might have affected the postoperative pain. Drahonovsky et al. [15] showed in their randomized prospective comparative study of vaginal hysterectomy (VH), LAVH, and TLH that LAVH resulted in a lower consumption of analgesics than TLH or VH. Kim et al. [10] evaluated the postoperative pain with the use of LAVH, whereas the authors performed TLH.
The etiology of postoperative pain is multifactorial. Etiologic factors associated with postoperative pain include neuropraxia of the phrenic nerves due to pneumoperitoneum, the type of insufflated gas, residual pneumoperitoneum, operative wound pain, direct tissue trauma from electrocoagulation and mechanical injury, and sociocultural and individual factors [16–19]. The current study was designed as a randomized prospective study at a single institution, and TLH was performed in the same manner in the two study groups. Therefore, operative wound pain mainly affected the results on postoperative pain in this study.
The limitation of movement due to the proximity of the laparoscopic instruments to each other during the procedure is considered a major weakness of SPLS. Using articulating instruments, single-port surgery can be more easily performed. However, surgeons should consider the additional costs for articulating instruments, a flexible scope, and related equipment. The TLH procedure can be performed in a relatively small uterus without any laparoscopic instruments specifically designed for single-port surgery.
We have performed SPLS for various gynecologic lesions without any articulating instruments. Based on our experiences, articulating instruments would be useful for traction of the uterus to divide uterine vessels and cardinal ligaments. A surgical field could be obtained by pushing the uterus with the RUMI uterine manipulator in the direction opposite that of dissection of cardinal ligaments, performed by a second assistant. Adopting a 30°, 5-mm endoscope and a high-definition camera provided sufficient vision for TLH without the use of a flexible scope. Because we used a 0° endoscope, the endoscope and the laparoscopic instruments were positioned parallel with each other, which caused a limited field of vision and a collision between the endoscope and the surgical instruments.
If a 30° endoscope is used for SPLS, it can be kept away from the laparoscopic instruments, and a wider range of vision can be provided. In addition, a 45-cm endoscope is useful for SPLS. A commonly used endoscope is 30 cm long. Thus, the 45-cm endoscope allows the head of the camera to be positioned 15 cm behind the operator’s hands, thereby preventing a collision between the camera and the operator’s hands. Although articulating instruments or a flexible scope can prove helpful in ligating uterine vessels in patients with a large uterus more than 12 gestational weeks in size, they are not always needed for SPLS-TLH.
We have already demonstrated in our previous study that single-port TLH is a feasible approach in terms of surgical outcomes despite technical difficulties. However, the previous study was not a comparative study, and the authors compared the surgical outcomes in SPLS with those of other researchers who performed conventional TLH.
The current study shows that single-port TLH and four-port TLH do not differ significantly in terms of surgical outcomes including operative times and EBL. Other researchers also have demonstrated that single-port approaches are comparable with conventional laparoscopic approaches in terms of surgical outcomes despite the limitation of movement [10, 11, 20]. The technical challenges in performing single-port laparoscopic surgery can be overcome by the surgeon’s experience.
In conclusion, single-port TLH is a feasible approach for the relatively small uterus and has operative outcomes comparable with those for four-port TLH. However, reduction in postoperative pain with the use of single-port surgery is not evident. Other potential benefits, including better cosmetic outcomes and faster recovery with single-port TLH compared with conventional TLH, should be evaluated in a future randomized prospective study.
References
Wu JM, Wechter ME, Geller EJ, Nguyen TV, Visco AG (2007) Hysterectomy rates in the United States, 2003. Obstet Gynecol 110:1091–1095
Johnson N, Barlow D, Lethaby A, Tavender E, Curr E, Garry R (2006) Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev CD003677
Pelosi MA, Pelosi MA III (1991) Laparoscopic hysterectomy with bilateral salpingo-oophorectomy using a single umbilical puncture. N J Med 88:721–726
Lee YY, Kim TJ, Kim CJ, Kang H, Choi CH, Lee JW, Kim BG, Lee JH, Bae DS (2009) Single-port access laparoscopic-assisted vaginal hysterectomy: a novel method with a wound retractor and a glove. J Minim Invasive Gynecol 16:450–453
Lim MC, Kim TJ, Kang S, Bae DS, Park SY, Seo SS (2009) Embryonic natural orifice transumbilical endoscopic surgery (E-NOTES) for adnexal tumors. Surg Endosc 23:2445–2449
Jung YW, Kim SW, Kim YT (2009) Recent advances of robotic surgery and single-port laparoscopy in gynecologic oncology. J Gynecol Oncol 20:137–144
Jung YW, Kim YT, Lee DW, Hwang YI, Nam EJ, Kim JH, Kim SW (2010) The feasibility of scarless single-port transumbilical total laparoscopic hysterectomy: initial clinical experience. Surg Endosc 24:1686–1692
Fader AN, Escobar PF (2009) Laparoendoscopic single-site surgery (LESS) in gynecologic oncology: technique and initial report. Gynecol Oncol 114:157–161
Breivik H, Borchgrevink PC, Allen SM, Rosseland LA, Romundstad L, Hals EK, Kvarstein G, Stubhaug A (2008) Assessment of pain. Br J Anaesth 101:17–24
Kim TJ, Lee YY, Cha HH, Kim CJ, Choi CH, Lee JW, Bae DS, Lee JH, Kim BG (2010) Single-port access laparoscopic-assisted vaginal hysterectomy versus conventional laparoscopic-assisted vaginal hysterectomy: a comparison of perioperative outcomes. Surg Endosc 24:2248–2252
Tsimoyiannis EC, Tsimogiannis KE, Pappas-Gogos G, Farantos C, Benetatos N, Mavridou P, Manataki A (2010) Different pain scores in single transumbilical incision laparoscopic cholecystectomy versus classic laparoscopic cholecystectomy: a randomized controlled trial. Surg Endosc 24:1842–1848
Bisgaard T, Klarskov B, Trap R, Kehlet H, Rosenberg J (2000) Pain after microlaparoscopic cholecystectomy: a randomized double-blind controlled study. Surg Endosc 14:340–344
Leggett PL, Churchman-Winn R, Miller G (2000) Minimizing ports to improve laparoscopic cholecystectomy. Surg Endosc 14:32–36
Poon CM, Chan KW, Lee DW, Chan KC, Ko CW, Cheung HY, Lee KW (2003) Two-port versus four-port laparoscopic cholecystectomy. Surg Endosc 17:1624–1627
Drahonovsky J, Haakova L, Otcenasek M, Krofta L, Kucera E, Feyereisl J (2010) A prospective randomized comparison of vaginal hysterectomy, laparoscopically assisted vaginal hysterectomy, and total laparoscopic hysterectomy in women with benign uterine disease. Eur J Obstet Gynecol Reprod Biol 148:172–176
Alexander JI, Hull MG (1987) Abdominal pain after laparoscopy: the value of a gas drain. Br J Obstet Gynaecol 94:267–269
Korell M, Schmaus F, Strowitzki T, Schneeweiss SG, Hepp H (1996) Pain intensity following laparoscopy. Surg Laparosc Endosc 6:375–379
Sharp JR, Pierson WP, Brady CE III (1982) Comparison of CO2- and N2O-induced discomfort during peritoneoscopy under local anesthesia. Gastroenterology 82:453–456
Vitale GC, Collet D, Larson GM, Cheadle WG, Miller FB, Perissat J (1991) Interruption of professional and home activity after laparoscopic cholecystectomy among French and American patients. Am J Surg 161:396–398
Chow A, Purkayastha S, Aziz O, Paraskeva P (2010) Single-incision laparoscopic surgery for cholecystectomy: an evolving technique. Surg Endosc 24:709–714
Acknowledgments
This study was supported by the Brain Korea (BK) 21 project for medical sciences, Yonsei University, and by a National Research Foundation of Korea grant funded by the Korean government (2009-0071158).
Disclosures
Yong Wook Jung, Maria Lee, Ga Won Yim, San Hui Lee, Ji Heum Paek, Ha Yan Kwon, Eun Ji Nam, Sang Wun Kim, and Young Tae Kim have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
Yong Wook Jung and Maria Lee equally contributed to this work as co-first author.
Rights and permissions
About this article
Cite this article
Jung, Y.W., Lee, M., Yim, G.W. et al. A randomized prospective study of single-port and four-port approaches for hysterectomy in terms of postoperative pain. Surg Endosc 25, 2462–2469 (2011). https://doi.org/10.1007/s00464-010-1567-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-010-1567-z